Home » Allogeneic Stem Cell Transplantation » Unrelated Cord Blood Transplantation
Unrelated Cord Blood Transplantation
Need Help in BMT?
Fill this form Below
This information is intended for patients or parents who are contemplating umbilical cord blood transplantation. It provides an overview of the procedure and outlines any potential risks or side effects. In some cases, individuals receive blood-forming cells from donated umbilical cord blood, which is collected from the umbilical cord and placenta following a baby’s birth. The stem cells undergo testing, typing, counting, and freezing until they are prepared for transplantation. While close matches in cord blood transplants are preferred, the risk of Graft Versus Host Disease is significantly lower compared to other types of transplants, despite a higher risk of infection.
What is cord blood?
Once a baby is delivered and the umbilical cord, which connects the mother to the baby, is severed, a small amount of blood remains in the blood vessels of the placenta and the section of the umbilical cord that is still attached to it. This surplus blood, known as placental blood or umbilical cord blood, is no longer necessary for the baby after birth. In the context of transplantation, when cord blood is obtained from an unrelated source, it is referred to as Unrelated Cord Blood Transplantation or UCBT. This implies that the recipient of the transplant is not genetically related to the cord blood donor, who is either the mother or the baby.
Why Might I Need a Cord Blood Transplant?
Cord blood has the potential to be utilized for stem cell transplants in the management of over 70 diseases. Leukaemia has been the most prevalent disease treated, with inherited conditions such as Sickle Cell Anemia (affecting red blood cells, the immune system, and specific metabolic abnormalities) following closely behind. Patients with Lymphoma, Myelodysplasia, and Severe Aplastic Anaemia have also undergone successful cord blood transplants.
Why is Cord Blood Used For Transplants?
Cord blood encompasses the essential components of blood, including red blood cells, white blood cells, platelets, and plasma. Moreover, it also contains stem cells that serve as a reparative mechanism for the body. Specifically, we are highly intrigued by the hematopoietic stem cells in cord blood, as they are responsible for generating blood cells. In comparison to bone marrow, cord blood is significantly more abundant in stem cells. To illustrate, a kilogram of bone marrow contains 300 million nucleated cells (NC), whereas 50 ml of cord blood contains 10 million NC per kilogram.
How is The Cord Blood Collected?
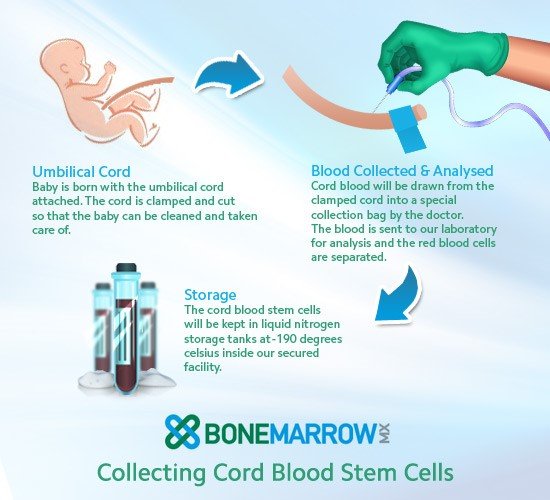
Cord blood is obtained from the umbilical cord of a newborn once it has been clamped. Both the placenta and the cord are considered waste materials post-birth and are typically disposed of. This process does not pose any risk to either the baby or the mother. Collection of cord blood is always done with the mother’s permission.
Whose Cord Blood Shall Be Used?
Parents, specifically the Mother, provide consent for the collection of cord blood from the Umbilical Cord post-delivery, along with the placenta. The cord blood units are donated voluntarily and stored in Public Cord Blood Banks without any upfront payment. Each cord unit undergoes screening and HLA typing, with the details being recorded in a centralized registry accessible to transplant centers globally. When a suitable match is found for a patient, the transplant center requests the specific cord blood bank to release the unit for transplantation, following the necessary criteria and paperwork from both parties. The transplant center is then invoiced for the cord blood unit, with charges ranging from 12,000 USD to 25,000 USD per unit. This process is known as ‘Unrelated Cord Blood Transplantation’.
Can I Store The Cord Blood of My Child For My Own Family?
The likelihood of utilizing one’s own cord blood for a personal transplant is exceedingly rare, with odds less than one in a million. In cases of urgent need, a child can provide bone marrow or peripheral blood for any family member over the age of 2. Consequently, the probability of using a cord blood unit for a family member remains equally slim. However, in families where a child is afflicted with conditions like Thalassemia or Leukemia and requires an immediate transplant, a cord blood unit from a newborn sibling, if a suitable match, can be utilized for the procedure.
This practice is known as ‘Directed Cord Blood Donation/Storage’. As medical professionals specializing in Bone Marrow Transplantation (BMT), we advise against private cord blood banking. Instead, we advocate for the donation of cord blood units to Public Cord Blood Banks to contribute to the pool of unrelated cord blood units accessible for BMT.
How Much Cord Blood is Needed?
Approximately 20 million nucleated cells per kilogram are required for successful engraftment of cord blood during transplantation. The likelihood of survival and recovery post-transplantation improves with a higher number of stem cells present in the blood. The quantity of cells necessary is dependent on the individual’s body weight, making umbilical cord blood transplantation more feasible in children and patients with lower body weight.
Is This Blood Safe?
After ensuring the well-being of both the mother and the family, cord blood is collected. Subsequently, the collected cord blood undergoes thorough testing in a laboratory to detect any presence of infectious diseases, including hepatitis and HIV. Only cord blood of excellent quality, devoid of any infections, is deemed suitable for transplantation purposes.
How Will a Match Be Found?
In contrast to other forms of stem cell transplantation, cord blood transplants do not require an exact match between the blood and the recipient. This process of matching is referred to as tissue typing or HLA matching. Nevertheless, it is understood that patients have a higher likelihood of a successful transplant and recovery when the match is more closely aligned.
Why is Cord Blood Important For People From Black And Minority Ethnic (BME) Backgrounds?
People from BME backgrounds have fewer matches in the bone marrow registry because:
- Individuals from ABME backgrounds are underrepresented in the Western countries where the majority of public cord blood banks are situated, resulting in a limited pool of potential donors.
- More than any other ethnicity, persons of Asian and African descent have different tissue types.
- Individuals of Asian and African descent have distinct tissue types.
Cord blood, unlike bone marrow, does not require as precise of a match, allowing it to be utilized in treating a broader range of individuals from diverse backgrounds.
What Are The Advantages of Using Cord Blood For a Transplant?
Cord blood offers benefits that surpass those of bone marrow and other stem cell sources for transplantation, such as:
- Lower incidence and severity of graft versus host disease (GVHD) – see under “Are there any risks or side effects?”
- Lower risk of viral contamination (similar to being polluted).
- More immediate availability.
- More flexibility; cord blood does not need to be a perfect match.
What Are The Disadvantages of Using Cord Blood For a Transplant?
Despite its abundance in stem cells, cord blood may not contain a sufficient amount of stem cells for certain larger patients. Cord blood transplants typically require a longer engraftment period. Additionally, if the initial transplant is unsuccessful, there is no option for a subsequent donation from the same source.
Are There Any Risks or Side Effects?
Despite being a recent development in India, cord blood transplants have been performed extensively in the USA and Europe. Similar procedures have also been conducted in countries like Japan and Australia. While all medical procedures carry inherent risks, the specific risks associated with cord blood transplantation will be outlined below.
- While the mother’s and the baby’s health are monitored during the cord blood donation process, there is always a chance of passing on a hereditary condition.
- Compared to bone marrow grafts or peripheral blood transplants, which take 10 to 14 days to engraft (take effect), cord blood transplants often take three to four weeks. Patients are more susceptible to infections during this time because they have less white blood cells, which are the body’s natural defense system. One way to characterize this is as having decreased bodily immunity.
General risk associated with transplantation are:
- Anaemia is a condition characterized by a decrease in the number of red blood cells in the bloodstream. This can result in weakness and may require blood transfusions until the body is able to produce an adequate amount of red blood cells again.
- Bleeding or bruising can occur when there is a decrease in the number of platelets, which are responsible for helping the body heal itself. Similar to anaemia, this can be treated with blood transfusions until the body is able to produce enough platelets.
- Infections are more likely to occur in the early phase after transplantation due to a weakened immune system. During this time, it is necessary to stay in the isolation room of the BMT unit. There is an increased risk of bacterial and fungal infections during this period. Once the white blood cells recover, the chances of these infections are reduced. However, there is still a risk of serious viral infections and other uncommon infections. These can usually be prevented through strict monitoring. Even after leaving the hospital, regular visits to the Day Care Unit for blood tests and examinations, typically twice a week, are necessary for monitoring purposes.
Graft versus host disease (GVHD): GVHD occurs when the lymphocytes, a specific type of white blood cell, in the transplant attack the recipient’s body. While it is typically mild and can be managed with medication, it has the potential to escalate into a more serious condition. Symptoms of acute GVHD may include:
- Diarrhoea
- Rashes
- Liver damage
Chronic GVHD can occur within three months following the transplant. This condition may present similar symptoms as acute GVHD, in addition to other manifestations.
- Dry eyes
- Sore mouth
- Joint pains
- Tightening of the skin
- Chest symptoms
Steroids and other medications are utilized to suppress the immune system in order to treat both acute and chronic GVHD.
Recurrence of the original disease: The success of the transplantation procedure, aimed at treating the underlying disease, is not guaranteed due to several factors.
- the stage of the disease
- response to previous treatment
- how many times the disease has recurred before transplantation.
Readmission: Hospital readmission may be necessary for the management of infections, GVHD, or other medical issues.
I Have Heard of Double Cord Transplantation – What Is It?
Physicians and scientists have commenced investigating transplants that involve cord blood from two distinct umbilical cords. The goal of dual cord transplantation is to enhance the recovery and longevity of patients. As of the end of 2013, around 5000 double cord transplantations have been performed in the USA, Europe, and Japan, resulting in positive outcomes despite a slight increase in GVHD. If you have any inquiries about double cord transplantation, please get in touch with BMTClinic.com.
What Happens Next?
It is crucial that you have a thorough understanding of the treatment process. Therefore, we encourage you to schedule an appointment with our specialists to discuss your case and address any inquiries you may have. Once it is determined that Cord Blood Transplantation is the appropriate treatment for you, our experts will outline the subsequent steps. Prior to any surgical procedure, you will meet with the surgeon and/or the anesthetist for another chance to seek clarification. Additionally, you will be required to sign a consent form.
Can Cord Blood Units Be Used To Cure Other Diseases Like Cerebral Palsy, Stroke or Spinal Cord Accidents, etc?
Cord blood contains a greater number of immature stem cells in comparison to adult bone marrow. The scientific community is actively engaged in studying and exploring the potential of these cells to repair damage in various organs. Nevertheless, it is important to note that this field of research is still in its early stages. At present, there is no substantiated proof indicating that directly infusing cord blood or bone marrow into an organ yields any significant benefits.
