Home » Identify the Donor
How To Identify The Donor For Stem Cell Transplant/ Bone Marrow Transplant

Who can donate stem cells for transplants?
During an Allogeneic Transplant, individuals receive healthy blood-forming cells from a donor, who can either be a family member or an unrelated individual. In some cases, patients receive donated blood-forming cells from umbilical cord blood, which is collected after a baby is born. The donor for a Bone Marrow Transplant (BMT) must be matched with the patient based on their tissue type, which is determined by typing their Human Leukocyte Antigen (HLA) antigens.
- Matched Related: In a family, the likelihood of finding a match in a brother or sister is approximately 25-30%. If no match is found within the immediate family, the chances of locating a fully HLA-matched donor among distant relatives are slim. Brothers and sisters are matched through a specialized test known as the Human Leukocyte Antigen (HLA) typing test.
- Matched Unrelated: The probability of finding a match with a random individual is less than one in a billion. However, by screening millions of people from similar ethnic backgrounds, a close match may be found. Volunteer-unrelated donor registries have been established in developed countries based on this idea, serving as the primary source of blood stem cells. Numerous registries worldwide offer over a million donors who are willing to donate marrow if necessary. The highest likelihood of finding a match is within the same ethnic community.
- Half-Matched/Haplo-identical: One set of HLA antibodies is inherited from each parent. As a result, parents and ourselves are never fully equal. Furthermore, there is a 90% likelihood that the patient’s siblings will be half-matched even if they are not entirely matched. BMT from a donor who is partly matched or haploidentical can be performed at centers with the necessary resources and experience. The only hospital in India with the necessary facilities and experience for this process is our Hospital and Research Centre. For patients who do not have a compatible donor, this is still their only option.
Stem cells can be derived from the donor’s bone marrow or peripheral blood, which refers to the blood in the veins. Alternatively, in certain instances, stem cells are harvested from the umbilical cord during the birthing process.
Human Leukocyte Antigen (HLA) Typing Test
Our team of specialists in Bone Marrow will assess whether an Allogeneic Transplant is the most suitable option for you, and we will initiate the process of identifying a suitable match. The matching process involves conducting Human Leukocyte Antigen (HLA) typing tests. Initially, the doctor will analyze the Patient’s blood to determine their HLA type.
HLA is a protein, or marker, present in the majority of cells in the body. The doctor will then search for a donor or umbilical cord blood that closely aligns with the Patient’s HLA. Our immune system utilizes HLA to distinguish between cells that are part of our body and those that are not. The most successful transplant outcomes occur when the Patient’s HLA closely matches that of the donor. A close HLA match also reduces the risk of complications post-transplant. Matching HLA markers is significantly more intricate than matching blood types.
A close match is important because it:
- Improves the chances of a successful transplant.
- Helps the patient’s donor cells engraft (grow and make new blood cells in the body).
- Reduces the risk of complications like graft-versus-host disease (GVHD). GVHD happens when the immune cells from the donated cells (the graft) attack the recipient’s cells (the host).


HLA Typing Test Kit And Sample Collection
If you are unable to access the High-resolution Human Leukocyte Antigen (HLA) Typing Test in your country, rest assured that you can reach out to BMTClinic.com for support at any time. In order to proceed with a Bone Marrow Transplant, it is essential to conduct Human Leukocyte Antigen (HLA) typing tests on the patient, siblings, and parents to determine the most suitable donor for the transplant.
There are two options:
- Upon arrival in India for the BMT procedure, the patient, siblings, and parents have the option to undergo HLA typing tests. However, the entire family needs to make the trip.
- Kindly share your contact information and home address with the BMTClinic.com team so that we may dispatch complimentary HLA Test Kits to your doorstep for the patient, siblings, and parents.
HLA Test Kit
The process of collecting samples for the HLA typing test is straightforward. Each HLA kit contains cotton swabs that are used to collect cheek cell samples from the inner mouth. Once collected, the samples should be securely packed and sent to us in India via courier service. To proceed with the test, a payment of 200 US dollars per kit should be transferred to our company account via wire transfer. Upon receiving the payment, we will ship the samples to reputable laboratories that conduct High Resolution HLA typing tests.
Alternatively, you have the option to send the HLA test samples directly to HISTOGENETICS Lab in the USA. In this case, a payment of 200 US dollars per kit should be transferred to their account via wire transfer.
Patient HLA Typing
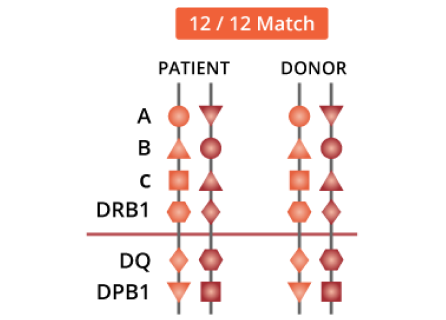
It is necessary to conduct HLA typing of the patient in a certified laboratory. Both the patient and the donor should undergo HLA typing using DNA methods, which should include HLA-A, -B, -C, and DRB1 as a minimum requirement. Serology can be used additionally to determine protein expression. It is recommended to include HLA-DRB3, DRB4, DRB5, and DQB1 typing, while HLA-DPB1 typing is optional. For HLA-A, B, and DRB1, it is preferable to have high-resolution typing.

Donor Selection
Donors for individuals in need of an Allogeneic Bone Marrow Transplant, regardless of their relationship to the recipient, are chosen according to various factors that have been shown to impact the patient’s prognosis.
- At least 5 of the 6 most significant “antigens,” which are the “A,” “B,” and “DR” antigens, and the donor and recipient’s HLA (tissue) types, should match closely. The donor and receiver should ideally match on all six antigens, and ideally, 10 out of 10 antigens—including 2 “C” and 2 “DQ” antigens—will match.
- Male or never-pregnant female matches are favored if a patient has more than one 10/10 match available.
In cases when there are numerous eligible matches, the youngest donor will typically be chosen; however, the selection will also take into account the donor’s health history and previous exposure to common viruses, including the CMV virus.
Testing Potential Donors
Testing for compatibility solely involves blood testing; a bone marrow test is not necessary to assess an individual’s suitability. To make sure they are the appropriate donor for the patient, potential donors must travel to India for testing.


Preliminary Donor Tests
All potential donors are required to undergo a series of pre-collection blood tests. These tests will encompass screening for hepatitis viruses and HIV (the AIDS virus), as well as urine tests. Additionally, a comprehensive medical history and physical examination will be conducted by a physician.
Donors who are 40 years of age or older may also be subjected to a chest X-ray and an electrocardiogram (ECG). In the case of donors undergoing a bone marrow harvest, an anesthetist will also evaluate their medical history, perform a physical examination, and discuss the anesthesia method. Typically, a general anesthetic is administered, although a spinal anesthetic (freezing from the chest down) may also be utilized.
Myths And Facts About Bone Marrow Donation
Find out the truth behind common false beliefs about bone marrow donation.
1. Donors Between the Ages of 18 and 44 Provide the Greatest Chance for Transplant Success.
Over 95% of the time, doctors ask for donors who are between the ages of 18 and 44. Age restrictions are not intended to be discriminatory. They are intended to safeguard the donor’s safety and give the patient the best potential outcome.
2. Patients are Most Likely to Match Someone of the Same Ancestry.
Increasing the number of individuals who contribute to the registry’s ethnic diversity broadens the range of tissue types accessible, assisting more patients in finding the match they require. We particularly need participants who identify as:
Members with these backgrounds are especially needed:
Black or African American
American Indian or Alaska Native
Asian, including South Asian
Native Hawaiian or other Pacific Islander
Hispanic or Latino
Multiracial
3. All Donors Are Carefully Prescreened to Ensure They Are Healthy and the Procedure Is Safe for Them.
Peripheral blood stem cells (PBSC) and bone marrow are the two donor options. The optimum donation method for the patient is determined by the patient’s physician.
PBSC donation is the most popular method of donation; it is a non-invasive process. You will receive filgrastim injections for 5 days before donation to boost the quantity of blood cells in your system that are utilized for transplantation. After that, a portion of your blood is drawn from you via an arm needle and sent through a machine to remove the blood-forming cells. You receive the leftover blood via the opposite arm. Watch the PBSC donation video to find out more.
Donating bone marrow is an outpatient surgical procedure. You won’t experience any discomfort throughout the donation because you will be given anesthesia. To remove liquid marrow from the rear of your pelvic bone, doctors use a needle.
While every medical procedure carries some level of risk, it is uncommon to experience any lasting side effects after donating PBSC or bone marrow. The body typically replenishes its cells within 4 to 6 weeks. Since only a small percentage (1 to 5% or less) of your marrow is required to potentially save a patient’s life, your immune system remains robust.
4. Donors Never Pay to Donate Marrow.
All medical costs for the donation procedure are covered by Registries or organizations or by the patient’s medical insurance.
5. Your gift saves lives.
Grow the registry of potential marrow donors
Help patients with crippling transplant costs
Advance the science of transplant
There are many ways you can help even if donation is not an option:
Fundraise
Host a drive
Volunteer
Spread the word

